HIV Pre-Exposure Prophylaxis (PrEP) Online Course at Coursera Review. Day 15 of 42.

In the third week of the PrEParing course, instructors will review the application of PrEP to people from vulnerable communities and high-risk groups: transgender people, MSM, adolescents, serodiscordant couples, victims of sexual violence, injecting drug users and commercial sex workers. This week will be very intense: for patients, content covers self-advocacy and population-focused concerns and resources for PrEP services; for providers, instructors will discuss the need and approach for tailoring PrEP for priority and often under-served communities with cultural humility.
The first lecture on the use of PrEP among transgender people was read by Dr. Deborah Dunn, from the Chase Brexton Health Services clinic. The Chase Brexton Clinic is known for being the world’s first gay clinic in 1978, the clinic is also one of the first in the world to face the HIV / AIDS epidemic, and Chase Braxton’s employees participated in the research and implementation of HIV treatment and prevention.
Dr. Deborah specializes in specialize in gender medicine for transgender and gender nonconforming people. Also, she was involved in the development of the «Gender JOY» program which serves the trans youth and families and hit over 700. Dr. Deborah says that younger patients are six years old, the age of the elders is approaching 80 years.
In this lesson, Deborah started discussing the coordination of medical care for transgender people, because transgender medicine has not yet been taught in any medical school in the world. Part of the discussion is hormonal therapy, but ethical issues and the individual approach to patients of different identities are often bypassed.
Studies in the US have shown that transgender people experience discomfort when they visit a doctor and often feel that a physician lacks knowledge of transgender medicine. Therefore, transgender people often do not attend to the doctor, not resolving health problems in time. Dr. Deborah Dunn advises paying attention to conferences, literature and scientific articles, evidence-based clinical guidelines on transgender medicine. A large number of such resources could be found on the website of the World Association of Health for Transgender People wpath.org. Deborah’s recommendation for transgender people is to find a doctor who is aware of the current state of science in the field of transgender medicine. This will allow transgender people to feel calm and confident while visiting a doctor.
So who are these transgender people?
Transgender people are people who have a gender identity or gender expression that differs from their assigned sex. It is postulated in gender theory that gender is not determined solely by the gender assigned at birth, but is determined by the feeling, conviction and final expression of a person’s opinion and identity. The goal of treating transgender people is to improve their quality of life by facilitating their transition to a physical condition that more closely reflects their sense of self.
Gender theory also proposes encouraging everyone to start looking at gender in a non-binary way:
- there’s no longer the male and there’s no longer the female;
- almost male;
- almost female;
- trying to be male;
- trying to be female;
- a male trapped in a female body;
- female trapped in a male body and other identities.
Such identities can be combined under the general term “gender-non-binary people,” although there may be definitions such as queer or gender-fluid.
It is important for a doctor and organizer of healthcare to understand the characteristics of communication with gender non-conforming people because such people often experience depression, a sense of social isolation. Deborah talks about the case when a doctor at the Chase Braxton clinic mistakenly called a transgender eight-grade girl a boy, and after that the girl committed suicide.
Therefore, PrEP provider should carefully consider the inner world of gender-nonbinary people. In the Chase Brexton Clinic of sexual health, Dr. Deborah suggests starting a dialogue with the question of what gender the patient is, how the patient is comfortable to be called — he, she or otherwise. If the patient has questions or misunderstandings, Deborah will specify what sex the patient was given at birth and what is the current identity. She recommends also ask a question about a person’s sexual orientation. If there was a change in gender identity in a person’s life, whether surgery and hormonal therapy were performed.
Such questions help Deborah asks to establish intimate contact with the patient. Also, the answers to questions about sexual history are essential for deciding about putting the patient on PrEP. Therefore, if it is difficult for doctors and medical personnel to ask questions about sexual orientation or gender identity, they could ask a patient to fill in printed form.
The Healthy People 2020 movement states that transgender people are at the top five health disparities due to discrimination, social and economic marginalization. Because of these concerns, transgender people are more likely to start using psychoactive substances, to be persecuted and abused, to have psychiatric illnesses, to experience suicidal thoughts, and up to 41% of transgender people report suicidal attempts.
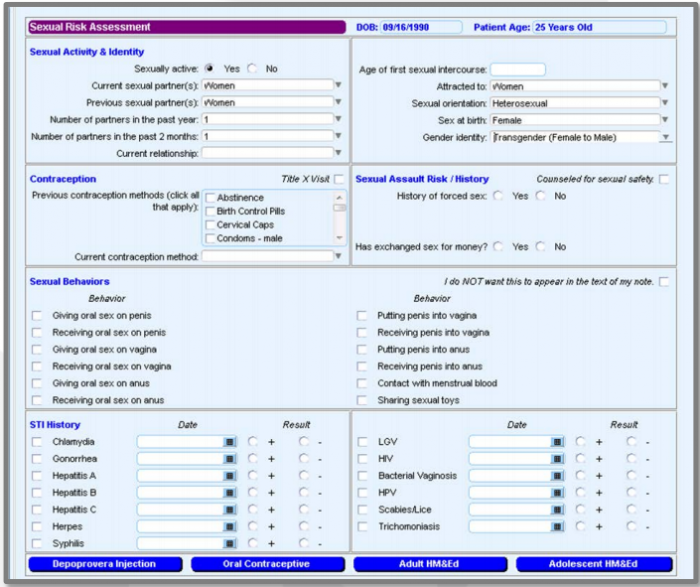
Figure 1 — Collection of patient information at the Chase Braxton Clinic
Dr. Deborah Dann recommends that you carefully fill out the medical records and shows how the collection of patient information at the Chase Braxton Clinic of Sexual Health is organized (Figure 1). The collection of medical information, supplemented by the results of the survey on sexual orientation and gender identity, helps to develop new public health programs that take into account the needs of all people in society.
It is important to use neutral words in the survey forms and in dialogues that will not allow the patient to feel uncomfortable or embarrassed:
- «partner» instead «husband» and «wife»;
- «parent» instead «mother» and «father»;
- in the «gender» field make is possible for a patient to write his gender sex, not only «male» and «female.»;
Deborah recommendeds also to pay attention to the overall design of the clinic:
- How do people describe the general feeling of entering the clinic and waiting for transgender people?
- Does visual communication in the clinic reflect the reality of transgender people’ life?
- Does the clinic have gender neutral restroom?
- How does the staff of the clinic communicate with transgender people?
The doctor continues to collect information with questions:
- How many sexual partners have you had in the past two months ?;
- What is your partner’s gender?
- What types of sexual activity does the patient practice?
- Does the patient involved in a monogamous relationship HIV-positive partner?
- What about condoms use?
When a doctor turns to questions about methods of protection during sex — it is important to use the moment to educate the patient. To do this, the doctor should have demonstration samples of latex napkins, condoms for vaginal, oral and anal sex, rings, gels in the office. If the doctor notices that the patient needs to be informed about the methods of prophylaxis, it is necessary to demonstrate how to apply it correctly.
HIV among transgender women
Recent studies have shown that transgender women are twice as likely to be exposed to HIV transmission as men who have sex with men (MSM). Black transgender women are more likely to transmit HIV.
The reasons for this high HIV prevalence among transgender women are drug abuse, promiscuity, marginalization, depression. Such people are often being rejected by their families, churches, employers, so they seek where they can find comfort — someone in alcohol or drugs, someone in promiscuous sex. They think about it, and they seek for a person who accepts them for who they are. Often they face conviction, insults, physical and psychological violence and even arrests in such a search.
Dr. Dunn says that more and more young transgender women are seeking help from year to year and she believes that HIV tests and counseling for PrEP should be offered to transgender people of any age if such people attend to a sexual health clinic. If it becomes clear from the dialogue with the patient that if this person is sexually active, it’s time to conduct a consultation and maybe provide PrEP, even if the patient is a very young age.
Transgender women can get HIV through the exchange of syringes with hormones or during illegal injections of silicone. Also in past lessons, instructors have already mentioned that the effectiveness of PrEP among transgender women is almost two times lower. Researchers test hypotheses about the interactions of PrEP with hormonal drugs. A study among HIV-positive transgender women in New York showed that they are less committed to taking antiretroviral therapy and are now they testing the hypothesis that adherence to taking PrEP among transgender women is also lower.
The lecture raised much more questions regarding the health of transgender women and men. Let us invite you to enroll the PrEParing course by the link https://www.coursera.org/learn/prep or ask questions in Life4me+ page on Facebook.
Stay with us and stay healthy!