HIV Pre-Exposure Prophylaxis (PrEP) Online Course at Coursera Review. Day 11 of 42.

The eleventh lecture of the PrEParing course “Community-Based Implementation of CDC PrEP Guidelines,” presented by Pierre-Cedric Crouch, the Director of Nursing at Magnet over at Strut — a project of the San Francisco AIDS Foundation.
Pierre-Cedric offered to talk about the CDC PrEP guidelines and applying them to a community-based clinic. The instructor also prepared to share his experience of providing PrEP in San Francisco.
Conflict of interests
Pierre-Cedric also reveals a conflict of interest. You could recall from the eighth lesson that disclosing a conflict of interest is beneficial for people listening to a scientific or popular science lecture since they get an exact state of science overview in the speaker’s area of competence. The narrative may be biased if the speaker reports on existing or past contracts with pharmaceutical companies.
The San Francisco AIDS Foundation, where Dr. Crouch works, does receive funding from the Gilead Sciences pharmaceutical company, but Dr. Crouch does not receive private grants from Gilead.
Gilead provides Truvada on the market — the only one approved by the US Food and Drug Administration (FDA) for PrEP. Therefore, the reader of this article understand that the instructor is potentially interested in promoting the drug, but as yet there are no alternatives — PrEP radically reduces a risk of HIV transmission, and the only available drug is Truvada.
Abbreviations
Next, would you mind recalling some abbreviations:
PrEP — pre-exposure HIV prophylaxis
nPEP — post-exposure HIV prophylaxis for people whose work is not associated with HIV (for everyone except doctors, nurses, laboratory staff, etc.)
MSM — men who have sex with men
MSW — men who have sex with women
WSM — women who have sex with men
IDUs — injecting drug users
STI — Sexually Transmitted Infections
PrEP clinical practice guidelines
Wolters Kluwer’s UpToDate, an evidence-based, physician-authored clinical decision support resource which clinicians trust to make the right point-of-care decisions, gives such a definition of the term:
Clinical practice guidelines are recommendations for clinicians about the care of patients with specific conditions. They should be based upon the best available research evidence and practice experience.
The Institute of Medicine defines clinical practice guidelines as “statements that include recommendations, intended to optimize patient care, that are informed by a systematic review of evidence and an assessment of the benefits and harms of alternative care options”.
Based on this definition, guidelines have two parts:
- The foundation is a systematic review of the research evidence bearing on a clinical question, focused on the strength of the evidence on which clinical decision-making for that condition is based.
- A set of recommendations, involving both the evidence and value judgments regarding benefits and harms of alternative care options, addressing how patients with that condition should be managed, everything else being equal.*
Over the past year, more than a dozen states announced free providing of PrEP among the citizens of these countries from high-risk groups.
Pierre-Cedric notes that clinical recommendations are not always universal. Developers of clinical guidelines tend to standardize PrEP, so that recommended practices to be convenient and safe in any community, but guidelines need to be adjusted locally. Further, Dr. Crouch will describe how the CDC clinical practice guidelines on prescribing PrEP were applied and improved in the Magnet-Strut clinic.
The Strut Clinic opened in San Francisco in January 2015 and offered sexual health care to gays, bisexuals, queers and transgender men, also providing psychotherapeutic assistance, substance abuse services, prevention of HIV transmission and various community engagement programs for people who are at risk for HIV or are already HIV-positive.
The clinic advises clients on the use of PrEP and provides the only approved drug for PrEP, a combination of emtricitabine and tenofovir Truvada. In the future, Strut hopes to expand the range of HIV preventing methods.
PrEP, according to the clinical guidelines of the CDC, is shown for:
-
men who have sex with men, MSM: If they are not in a monogamous relationship with an HIV-negative man, there has been sexual contact in the last six months AND at least one of the conditions:
- was anal sex without a condom in the last six months;
- was diagnosed with STI in the last six months;
- are in an ongoing relationship with an HIV-positive man;
-
men who have sex with women, MSW: If they are not in a monogamous relationship with an HIV-negative woman, there has been sexual contact in the last six months AND at least one of the conditions:
- had sexual intercourse with both women and men in the last six months;
- infrequently uses condoms during sex with 1 or more partners of unknown HIV status who are known to be at substantial risk of HIV;
- is in a ongoing relationship with an HIV-positive woman.
-
women who have sex with men, WSM: if they are not in a monogamous relationship with an HIV-negative man, there has been sexual contact in the last six months AND at least one of the conditions:
- during sexual intercourse for the last six months, the male partner did not use a condom or did not always use a condom, and the HIV status of this partner is unknown, or the partner is at a substantial risk for HIV;
- is in an ongoing relationship with an HIV-positive man.
The doctor prescribes PrEP only if a person is at substantial risk of getting HIV.
For injecting drug users, IDUs, PrEP is prescribed in cases where at least one of the following conditions is met:
- injecting drugs have not been prescribed by a doctor for the last six months (if not prohibited by local law) AND for the last six months, at least one of the following conditions has been met:
- any sharing of injection or drug preparation equipment in past six months;
- been in a methadone, buprenorphine, or suboxone treatment program in past six months;
- risk of sexual acquisition;
Such guidelines seem logical and consistent, but practical application causes difficulties — in fact, the doctor determines a small category for each client and decides on this — whether to prescribe PrEP or not. However, people are different, and therefore Dr. Crouch shares the experience of the Magnet program in San Francisco. The ultimate goal for the doctor is to determine for every client if there is a substantial risk of getting HIV.
Therefore, in Magnet, doctors expand indications and prescribe PrEP to each person who reported an episode of sex without a condom in the last year. Also, PrEP is prescribed to those whose partner is HIV-positive, although the new data say that if the HIV-positive partner has undetectable viral load, then the risk of HIV transmission in the couple is extremely low. CDC researchers are planning to review recommendations for HIV-negative people who live in conjunction with HIV-positive in the new version of the clinical guidelines for PrEP.
Also, doctors in Magnet prescribe PrEP to patients who are injecting drug users and at least once shared a syringe in a past year. The Magnet project distributes clean needles so that the staff will give to such patients clean needles; this practice reduces the risk of transmission of HIV and hepatitis C.
PrEP is also provided for someone with a low-risk of exposure to HIV if in an interview such a person will tell about the possible risky behavior in the future.
Clinical Evaluation and Counseling
The CDC recommends that doctor should get a negative HIV antibody test within the last seven days, and also assess for signs of acute HIV infection. These include fever, fatigue, muscle pain, lymph nodes enlargement, skin rashes, sore throat. And for people who actually might have had a recent exposure to HIV, they should be offered PrEP.
PrEP is prescribed if the HIV test is negative, there is no evidence of acute HIV infection, and the client has a substantial risk of getting HIV in the future.
The doctor also needs to have a recent eGFR greater than 60 and to do Hepatitis B and Hepatitis C serologies as well.
eGFR is short for estimated glomerular filtration rate. Your eGFR is a number based on your blood test for creatinine, a waste product in your blood. It tells how well your kidneys are working.
The eGFR is a useful test, but it’s not right for everyone. For example, this test may not be accurate if you are younger than 18, pregnant, very overweight or very muscular.
Definition from the American Kidney Fund website
Hepatitis C is not contraindicated for PrEP; The test is made as part of a routine, a sort of panel just to see if there is Hepatitis C. If someone does have Hepatitis C, the doctor could prescribe them PrEP without modifying anything.
If someone has Hepatitis B, the doctor would need to ensure that this client getting Hepatitis B treated accordingly. Some of the clients can have Hep B, and Hep C at the same time, they just need a little extra medical evaluation to treat their Hep B alongside receiving PrEP.
Next, clients receive PrEP and adherence counseling, but at Magnet they just a little bit more:
- an HIV antibody test within seven days;
- assessment for acute HIV infection having benefit to access to an HIV RNA test which helps narrow the window of exposure for HIV;
- a renal and metabolic panel on all clients;
- Hepatitis B antigen and Hep C antibody testing;
- a significant amount of PrEP and adherence counseling;
- gonorrhea, chlamydia, and syphilis testing;
- detailed benefits navigations.
Early start of prevention
Starting people up on the same day in the Magnet-Strut clinic is possible, there is enough testing out there and access to provide people with PrEP that same day, says Dr. Crouch. The clinic is equipped with laboratory equipment thanks to the grants from the San Francisco AIDS Foundation, so the tests are performed during the client’s visit in one place. Recent research, like iPrEx OLE in 2014, led the organizers of the clinic to understand that the long delays just end up frustrating clients and prolongs their risk of HIV, so getting people on PrEP as soon as possible is vital.
In the iPrEx, OLE study scientists proposed to invite everyone who they all met to put on to PrEP to answer the questionnaire that would reveal an acute retroviral syndrome among the respondents.
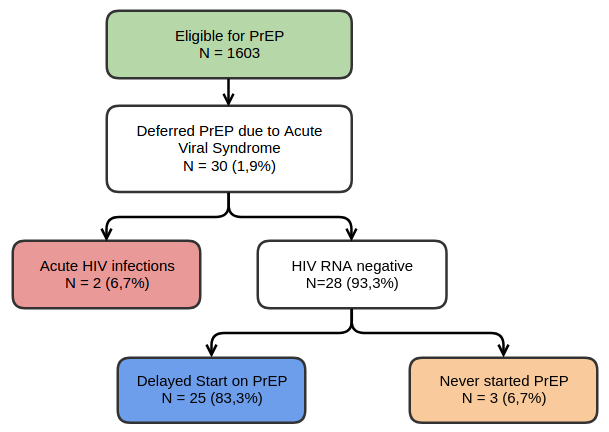
Figure 1 — Clinical Screening for Acute Viral Syndromes and Acute HIV Infection in iPrEx OLE. Source: Grant et al, Lancet ID, 2014.
As seen in the diagram (Figure 1), the study involved 1,603 people, 30 of them showed signs of an acute retroviral syndrome, usually observed in the first weeks of HIV infection, that put up a red flag delaying the initiation of PrEP. Such people were offered to perform blood analysis for HIV, not an express test, but an expensive PCR test for HIV RNA. Two people showed an acute phase of HIV infection. Among the remaining 28 subjects, 25 started the PrEP with a delay, and three people abandoned the PrEP.
Pierre-Cedric made three conclusions from the iPrEx OLE study results:
- it is necessary to conduct a survey of those who applied for PrEP to identify signs of possible acute HIV infection of the early phase and, in a case of HIV, offer such people an early start of treatment;
- delay in putting on PrEP leads to the fact that some people disappear and do not start PrEP while having a substantial risk of exposing to HIV and have all the indications to PrEP;
- skilled management of the clinical process makes it possible to identify people with an acute phase of HIV infection whereas to provide the bulk of clients with PrEP right on the day of visit;
Kidney function evaluation
When doctors talk about evaluating kidney function in a patient, they most often mean estimating the glomerular filtration rate — an indicator of the kidneys’ effectiveness in purifying blood from creatinine and removing it from the urine. This test shows the ability of the kidneys to cleanse from harmful substances.
This indicator does not always give an adequate picture — if the client is under 18 or dehydrated or brawny or takes ibuprofen or exercised before the test or took a nutritional supplement with creatinine — the results will be biased. In such cases, the doctor will try to avoid the risk of kidney damage and possibly will not prescribe PrEP to such a client.
Therefore it is important to do repeated tests, but there are also alternative ways of estimating kidney function. Doctors at Magnet use a new diagnostic test with the Cystatin C protein. The results of evaluating kidney function based on the level of cystatin C give a clearer picture.
“You don’t want not to start someone on PrEP just because they have a high creatinine that has nothing to do with their kidney function at all,” says Pierre-Cedric.
PrEP counseling
In Magnet clinic, doctors start off with three lead questions:
- What have you heard about PrEP?
- That helps them figure out all the different urban legends that people have around PrEP, and help correct those.
- What do you want PrEP to do for you?
- It’s a preferred question in the Magnet clinic; it allows to understand what people want from PrEP, whether the clinic solves the difficulties of clients. And what can be changed in the process to meet people expectations.
- What have you heard about the PrEP and condoms?
- The answer helps to understand the client’s sexual behavior and to help him to develop such a behavior for the future, so that a person really is protected from HIV. Often consultants asking clarifying questions:
- What does the relationship with condoms look like?
- Do you love them?, Do you hate them?
- Is it easy for you to use condoms?
- How’s that going to look like when you actually start up on PrEP?
- the idea is a doctor come up with a client centered sexual health plan that they develop with the help of a client.
PrEP adherence counseling
Dr. Crouch goes on to describe the adherence to PrEP counseling. Irregular intake of tablets during PrEP carries many risks to the client’s health along with people with having sexual relations with the client. Everything goes well if the tablets are taken accurately, but if you skip the reception — PrEP stops working, and the prophylaxis process is more complicated than “switch on — switch off.”
Therefore, in Magnet they offer consultations, discussing with each client:
- When to start PrEP and at what time and on what day the client is going to take the first pill;
- If a person missed one dose or seven doses — how to handle these sort of gaps. When to restart and what to do?
- Doess it easy to take PrEP at home?
- Does the client live with parents at home and if it possible to take PrEP when parents are at home?
- Does the client live with a partner who does not know about receiving PrEP?
- Other issues related to the possible stigma in client’s life and how to avoid stigma.
PrEP Navigation
US Public Health organizations have developed a “PrEP-navigation” program.
PrEP Navigation is to improve recruitment, linkage, and retention to care and health outcomes for people of color living with HIV or at high-risk for HIV. The program is based on the concept that persons in communities trained as HIV and PrEP navigators can be effective in reducing and eliminating barriers to the appropriate prevention, diagnosis, and treatment of HIV in their own communities.
Dr. Crouch says that participation in the PrEP Navigation is essential, especially if you’re not in a single payer system. In the Magnet program, they have an entire PrEP team that does everything for the client. They became trained notaries and insurance enrollment counselors, so they’re able to get all the documents signed and filled out for the clients. The majority of the time the client just signs a form, and they don’t have have to fill out anything. Filling out forms is a huge barrier to accessing care so Dr. Crouch recommends looking into those different options to educate benefits Navigation team to provide as much service as they possibly can.
PrEP follow up
Pierre-Cedric refers again to the CDC guidelines for PrEP, which recommends every person on PrEP taking an HIV test every three months. Also making pregnancy test for women during a visit, consulting on adherence, and monitoring possible side effects. Once every six months, it is recommended evaluating the kidney function and making a serology for syphilis, gonorrhea, and chlamydia.
So in Magnet, they slightly complement the CDC guidelines:
- Consultant calls client in the first three days after putting on PrEP, to ensure there are no problems accessing the pills in the pharmacy, or any insurance issues and whether the person does not feel any side effects;
- The first visit is appointed one month after PrEP started;
- Next visits are arranged every three months;
- During each visit, clients are tested for HIV, not an express test, but precise PCR for HIV RNA, which quickly identifies the virus during the “serological window”;
- STI analysis during each visit if necessary;
- Making sure that clients are not going to have any lapses in insurance to avoid breaks in PrEP intake;
- A test for Hepatitis C once a year;
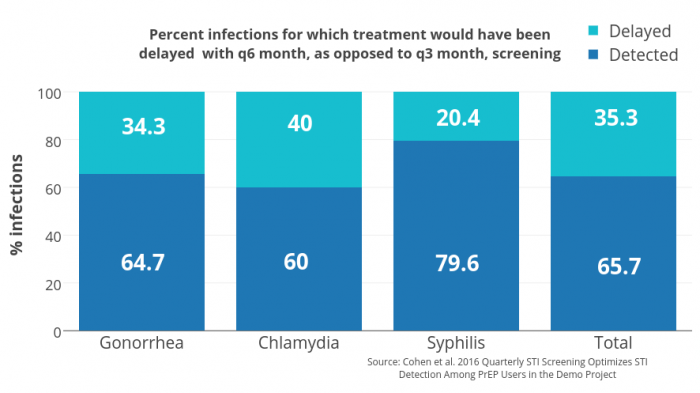
Figure 2 —Quarterly STI Tests: delayed and detected. Source: Cohen et al. 2016 Quarterly STI Screening Optimizes STI Detection Among PrEP Users in the Demo Project
STI tests are made more often than recommended by the CDC, as the clinic offers PrEP to people with high sexual activity. On the graph (Figure 2) presented by Dr. Stephanie Cohen of the San Francisco Department of Public Health, you could see how many bacterial infections are missed when clients tested every six months — a diagnosis and treatment of 20% −40% of STIs was delayed.
The later doctors diagnose an STI, the higher the chances of transmitting this infection to other people. Pierre-Cedric supplements these statistics — even when testing for STIs during the first visit after starting PrEP, doctors find a substantial amount of infections.
So Dr. Crouch encourages you to think that there might be some clients who need to get tested every month, depending on their risk factors. So really you want to tailor this to the client and also encourage more frequent testing, and not wait every six months to test somebody.
Therefore, the instructor says, the clinical recommendations are good, but they need to be personalized. It is not necessary to do an analysis on STIs every three months to a person who reliably lives in a monogamous partnership, and vice versa someone from a high-risk group should be invited to perform monthly blood tests.
Clinical practice guidelines for PrEP are available for download at the US Centers for Disease Control and Prevention website — https://www.cdc.gov/hiv/pdf/prepguidelines2014.pdf
This overview of the lecture “Recommendations for the introduction of PrEP in the community” came to an end. The lecture turned out to be voluminous, saturated with information. I hope you found it useful. We thank Dr. Pierre-Tsederik Kruch and the entire PreParing team from the Johns Hopkins University, as well as the Coursera online education platform.
This overview of the lecture “Community-Based Implementation of CDC PrEP Guidelines” came to an end. The lesson turned out to be some tricky, but we hope you found it useful. Let us thank Dr. Pierre-Cedric Crouch and the PrEParing course team from the Johns Hopkins University, as well as the Coursera online education platform.
We are waiting for you tomorrow at the lecture “PrEP Pipeline,” which will introduced by the woman you already know, Dr. Neha Pandit from the School of Pharmacy of the University of Maryland.
If you have not already signed up for the PrEParing course on the Coursera platform — it’s never too late. Just go to https://www.coursera.org/learn/prep.
Stay with us and stay healthy!